THYROID GLAND

ANATOMY OF TYHROID GLAND
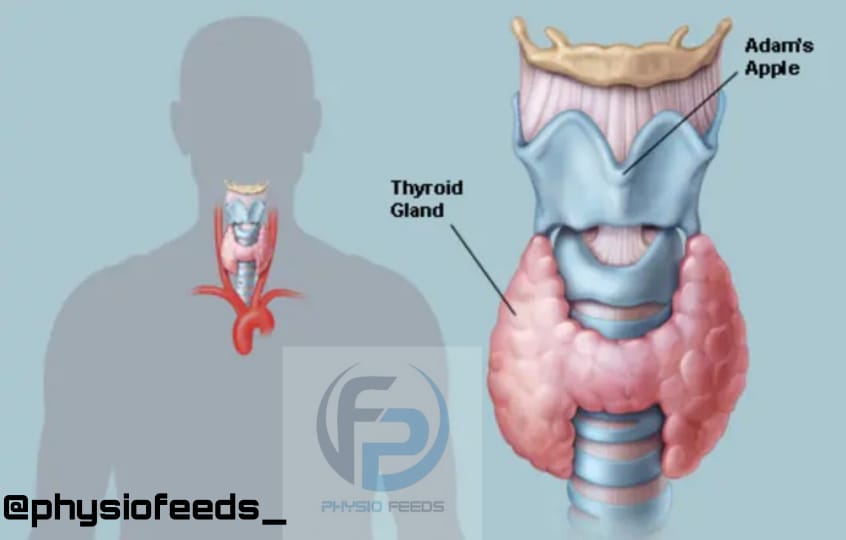
– Thyroid gland is an endocrine gland present in lower part of front and sides of neck.
– It regulates basal metabolic rate and has a important role in the calcium metabolism.
– It is roughly H shaped and It has 2 lobes and a isthmus.
* Situation and extent
– Gland lies against the C5, C6, C7 and T1 vertebrae.
– Each love extends from middle lobe of thyroid cartilage to fourth or fifth tracheal rings and Isthmus extends from second to third tracheal rings .
* Dimensions and weight
– Each lobe is measures about 2 inches ( length ) , one inch ( breadth ) and one inch ( thickness).
– The isthmus is 1/2 inch × 1/2 inch . And gland weighs about an average about 25g.

* Capsules
– It has a true capsule and a false capsule.
* Blood supply
– It has superior and inferior thyroid arteries.
• Superior thyroid artery : It is a branch of external carotid artery and supplies upper 1/3 rd of lobe and upper half of isthmus.
• Inferior thyroid artery : It is a branch of thyroid cervical trunk from subclavian artery.
It supplies lower 2/3 rd of lobe and lower half of isthmus.
* Venous drainage
– It has 3 veins
(1) Superior thyroid vein
(2) Middle thyroid vein
(3) Inferior thyroid vein.
* Structure and function
– It has 2 types of secretory cells : follicular and parafollicular cells
– The follicular cells secretes tri-iodo thyronine and tetra-iodo-thyronine.
– This stimulates basal metabolic rate and somatic and psyclic growth of individual.
– The parafollicular cells secretes thyrocalcitonine .
• Applied anatomy
– Goiter : any enlargement in thyroid gland
– Hyperparathyroidism
– Hypothyroidism.
• THYROID HORMONES
– There are 3 types of thyroid hormones
(1) Tetra-iodo-thyramin ( T4) / thyroxin
(2) Tri-iodo-thyramin ( T3)
(3) Calcitonin.
PHYSIOLOGY OF THYROID HORMONE
• Synthesis of T3 and T4
– These are produced by thryoid follicles.
– Thyroid follicles are made up of aceni which has a single layer of epithelial cells in centre.
– And it is filled with protein called as a colloid.
• Steps of thyroid hormone synthesis

1) Iodine trapping
– Iodide is present in the blood which is consumed in diet as iodine.
– When it passes through the thyroid gland it is actively taken up and is converted into iodide in acinar cells of thyroid gland.
2) Oxidation
– Iodine inside the cell is gets oxidised again back to iodine.
3) Organification
– Iodine binds with thyrosine and attached to thyroglobulin
– When the 2 molecules of iodine combined with thyrosine it forms diiodothyrosine.
– When only one molecules of iodine is combines with thyrosine it forms monoiodothyrosine.
4) Coupling
– After the formation of diiodothyrosine and monoiodothyrosine , the two molecules of diiodothyrosine is combined to form T4 and one molecule of monoiodothyrosine and one molecule of diiodothyrosine combines to form T3.
5) Release of T3 and T4
– After the formation of T3 and T4 in colloid hormones along with thyroglobulin is taken into acinar cells.
– Lysozymes in the cell releases T3 and T4 from thyroglobulin and then T3 and T4 is released into blood.
– Thyroglobulin is recycled for further hormonal production.
• Functions or actions of thyroid hormone
1) Calorigenic action
– Thyroid hormone increases activity of sodium – potassium pump and there by stimulates BMR.
2) Effects on metabolism
– Carbohydrate metabolism
– Protein metabolism
– Lipid metabolism
– Vitamin metabolism
3) Effects on blood
– Stimulates erythropoiesis hence increase RBC and increase blood volume.
4) On Cardiovascular system
– Increase heart rate
– Increase force of contraction
– Increase cardiac output
– Increase SBP
– Decrease DBP
5) Effects of respiratory system
– Increase respiratory rate
– increase force of respiration
– Increase demand of oxygen
6) On GIT
– Increase Appetite and hunger
– Increase GIT secretion
– Increase GIT motility
7) On CNS
– Thyroid hormone is essential for fetal growth.
– Lack of thyroid hormone during intra uterine life produces mental retardation.
– Thyroid hormone increases blood flow the brain and maintains normal Function of brain .
8) Effects on skeletal muscles
– thyroid hormones are protein catabolic hormones
– They Decrease size and bulk of skeletal muscle
9) Effect on sleep
– Decreases sleep
10) Effect on Reproductive system
– Increases metabolic rate in reproductive system
– In females excess thyroid hormones produces oligomenoria
– In males , excess thyroid hormones produces impotence,
11) Effect on other endocrine glands
– Stimulates activity of endocrine gland.
12) On growth
– Stimulates bone growth and skeletal growth before puberty .
PATHOPHYSIOLOGY
• HYPERTHYROIDISM
– Increased secretion of thyroid hormone is called as Hyperthyroidism.

* Causes
1) Grave’s disease : primary
2) Thyroid adenoma : secondary.
• Grave’s disease
– It is an autoimmune disease.
* Pathology
√ B – lymphocytes produces autoimmune antibodies ( thyroid stimulating autoantibodies )
√ They start acting like TSH
√ Hypersecretion of thyroid hormone
√ Thyrotoxicosis
• Signs and symptoms
1) Eye
– Exoptalmus proptosis ( protrusion of eye balls due to edematous swelling of retro-orbital tissues leading to optic nerve damage )
– Patient is unable to close eye
– Can lead to dryness of cornea
– Infection , ulceration
2) CVS
– Tachchycardia
– Hypertension
– Increased BP
– Arrythmia
– Cardiac failure
3) GIT
– Hypermobility of intestine which causes vomiting and diarrhea
4) Muscles
– Increase muscular weakness
– Edema over skin bones
– Whitish discolouration of skin
– Hair loss
5) CNS
– Nervousness
– Insomnia
– Mild tremor
– Anxiety
– Heat intolerance
6) Oligomenorrhea / Amenorrhea in females
* Investigation
1) Thyroid function test
– T3 , T4 is increased
– TSH is decreased
2) Detection of autoantibodies against thyroglobulin
3) Radioactive iodine uptake is increased
4) Fine needle aspiration
– Hyperplasia of thyroid cells
* Treatment
1) Anti-thyroid drugs
– Helps to suppress production of thyroid hormone
– Carbimazole
– Methimazole
2) Beta – blockers
– To relieve Tachycardia and heart rate
3) Radioactive iodine
– Destruction of functional thyroid cells
– Nitrates
– Thiocyanates
4) Surgery
– Thyroidectomy
* Secondary hyperthyroidism
– Thyroid adenoma
– Sometimes , a localized tumor develops in the functional thyroid cells ( thyroid adenoma ) which secretes large quantity of thyroid hormone.
– Depresses the production of TSH.
•HYPOTHYROIDISM
– Decreased secretion of thyroid hormone is called as hypothyroidism.
– Primary hypothyroidism : Decreased function of thyroid gland.
– Secondary hypothyroidism : Decreased secretion of thyroid hormone.

• MYXEDEMA
– Hypothyroidism in adults.
– Life threatening complication of hypothyroidism.
– Patient goes in state of coma.
• Pathophysiology
– Deposition of myxedematous tissues of various organ.
– Responsible for organ dysfunction

* Causes
1) Disease of thyroid gland
2) Iodine deficiency.
3) Deficiency of TSH
4) Auto immune
5) GI bleeding
6) Trauma or physical stress
7) Use of sedative diuretics.
*Signs and symptoms of MYXEDEMA
1) Edematous appearence throughout the body
2) Moon face
– Swelling of face
– Bagginess under eyes
– puffiness of face
– Non-pitting type of edema
3) Atherosclerosis
4) Arteriosclerosis
* General features
1) Tierdness
2) Weight gain
3) Frog like husky voice
5) Skin – Dry skin
Thick and rough
6) CVS – Bradycardia
Hypotension
Cadiac failure
7) CNS – Depression
Cold intolerance
8) Muscle – Stiffness
9) GIT – Constipation
10) Hematological
– Iron deficiency anemia.
– Pernicious anemia
– Decrease RBC synthesis
11) Reproductive – Menorrhagia
Infertility
Impotence.
* Investigation
√ Thyroid function test
– T3 and T4 decreases and TSH increases.
√ Radioactive iodine uptake decrease
√ Fine needle aspiration
– decreased thyroid cells.
* Management
– Replacement therapy
– Thyroxine therapy
– Supplementation of thyroid hormone.
• CRETINISM
– Hypothyroidism in children .

* Causes
– Congenital absence of thyroid gland
– Genetic disorder
– lack of iodine in diet.
* Features of Cretinism
1) At the time of birth , a newborn baby with hypothyroidism may appear normal because Thyroxine has been supplied from mother.
-But after weeks baby starts developing sluggish movements and croaking sound while crying .
– If not treated early , the baby will be mentally retarded permanently
2) Skeletal growth is affected more than the soft tissues.
– Bloated body.
– Tongue becomes big and there is a dripping of saliva.
– Obstruction in swallowing and breathing.